Written By: Ellen Osborn
Edited By: Jennifer Baily
Considering the massive media fever surrounding the current coronavirus outbreak, it might come as a surprise that most people are infected by one, if not multiple, coronaviruses during their lifetime. However, the current coronavirus outbreak is much more than just another flu.
Coronaviruses are a large family of viruses, of which several members cause mild to moderate upper-respiratory tract illnesses in humans, which account for 10% to 30% of these types of infections in adults. These endemic human coronaviruses (HCoVs) are considered inconsequential pathogens incapable of causing global epidemics. Until the early 2000s, HCoVs received little attention.
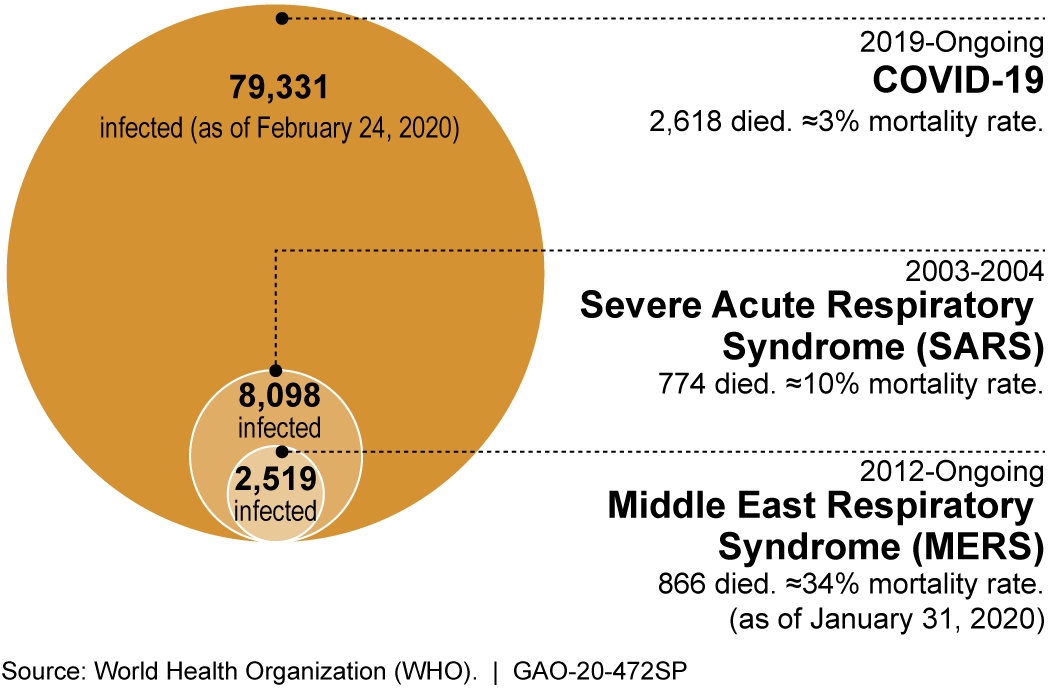
Figure 1: The recent outbreaks of coronavirus-caused diseases known to infect humans (COVID-19 numbers are confirmed and as reported by China).
This changed when two novel coronaviruses (nCoVs) jumped from their animal reservoirs into humans and caused the Severe Acute Respiratory Syndrome (SARS) outbreak in 2002 and then Middle East Respiratory Syndrome (MERS) outbreak in 2012. Together, the SARS coronavirus (SARS-CoV) and MERS coronavirus (MERS-CoV) resulted in over ten thousand confirmed cases and 1640 deaths. The international panic brought about by these coronavirus outbreaks was crippling. In response, the World Health Organization (WHO) placed SARS-CoV and MERS-CoV on its Priority Pathogen list in an effort to galvanize research into nCoV biology as well as providing countermeasures to contain future outbreaks.
Just two years later, an outbreak of an nCoV began in Wuhan, China. This nCoV is officially named SARS-CoV-2 due to preliminary analyses that identified genetic similarities to the 2002 SARS-CoV. Because the official name references SARS, the WHO shortly began referring to the virus as “the virus responsible for coronavirus disease 2019 ,” or COVID-19, in order to prevent unnecessary panic in populations affected by the 2002 SARS outbreak.
The strong similarities between the COVID-19 coronavirus and SARS-CoV will undoubtedly assist in preventing and treating COVID-19. However, coronaviruses remain one of the least understood family of viruses due to their exceptionally large genome and proteome, and as a consequence, the complexity of the virus’ interactions with hosts. Here at the University of California, Davis, the California National Primate Research Center and Center for Immunology and Infection Diseases are working to establish a rhesus macaque model of COVID-19, which will be fundamental in understanding viral dissemination and age-related differences in COVID-19 disease progression. Additionally, the Interdisciplinary Research & Strategic Initiatives division of the Office of Research is coordinating the campus’ response to COVID-19 research funding opportunities and established the UC Davis COVID-19 Research Working Group to enable efficient sharing of resources, information, and to connect potential collaborates across UC Davis.
As an average news consumer, it has been difficult to pinpoint the exact level of concern COVID-19 merits. At the beginning of March, the WHO recorded 127 cases of COVID-19 in the United States – nine of which were fatal – and that community spread was beginning to occur in several locations. The CDC also received heavy blowback for an uncharacteristically slow response and subsequent release of a faulty test kit. Is the United States destined for an uncontrolled spread of coronavirus? Some are saying no and point to a more encouraging trend emerging from China in recent weeks. Dr. Bruce Aylward, an expert from the WHO, recently returned from a two-week trip to China to assess the state of the coronavirus outbreak after the country’s initial response garnered a storm of anger from its citizens and the rest of the world and relayed optimistic data. At the end of January, China was diagnosing over 2000 new cases per day with 31 provinces on red alert, but by early March, there were less than 100 new cases per day with 24 provinces down to yellow or green alert. Dr. Aylward says that this data is a good sign, and that with appropriate government-sanctioned public health measures and public cooperation, COVID-19 can still be contained globally, despite less than encouraging initial government responses.
Other world leaders and health professionals are suspect of China’s severe approach to contain COVID-19, questioning the effectiveness of essentially putting hundreds of millions of people, regardless of their health, on house arrest. Michael T. Osterholm, director of the Center of Infectious Disease Research and Policy at the University of Minnesota, wrote in a recent New York Times op-ed that although China did a remarkable job of slowing the progress of the outbreak, he is not convinced that it is sustainable and asks what others are asking: did the Chinese actually contain the virus, or have they just suppressed it? Only time will tell whether the virus will continue to spread when the Chinese people return to work and school. Even if the virus was successfully contained, it is hard to believe that China’s cordon sanitaire* could be reproducible in other countries that do not have the same surveillance infrastructure as China and whose citizens are not accustomed to authoritative government action.
Though the data are incomplete and public health measures in the United States have yet to be fully formed and delivered, it seems fair to say that social distancing is essential to contain COVID-19. Containment might require people to make sacrifices they are unaccustomed to, like working from home and canceling social events, but these are ultimately small sacrifices in the face of a global pandemic. In the meantime, instead of trying to gauge how concerned we should be from the headlines, it might be better to take the advice of New York Times reporter Donald McNield who has covered disease outbreaks since 2002: “don’t panic; watch the data.” As graduate students, we are uniquely qualified to practice this advice and communicate the data to our community.
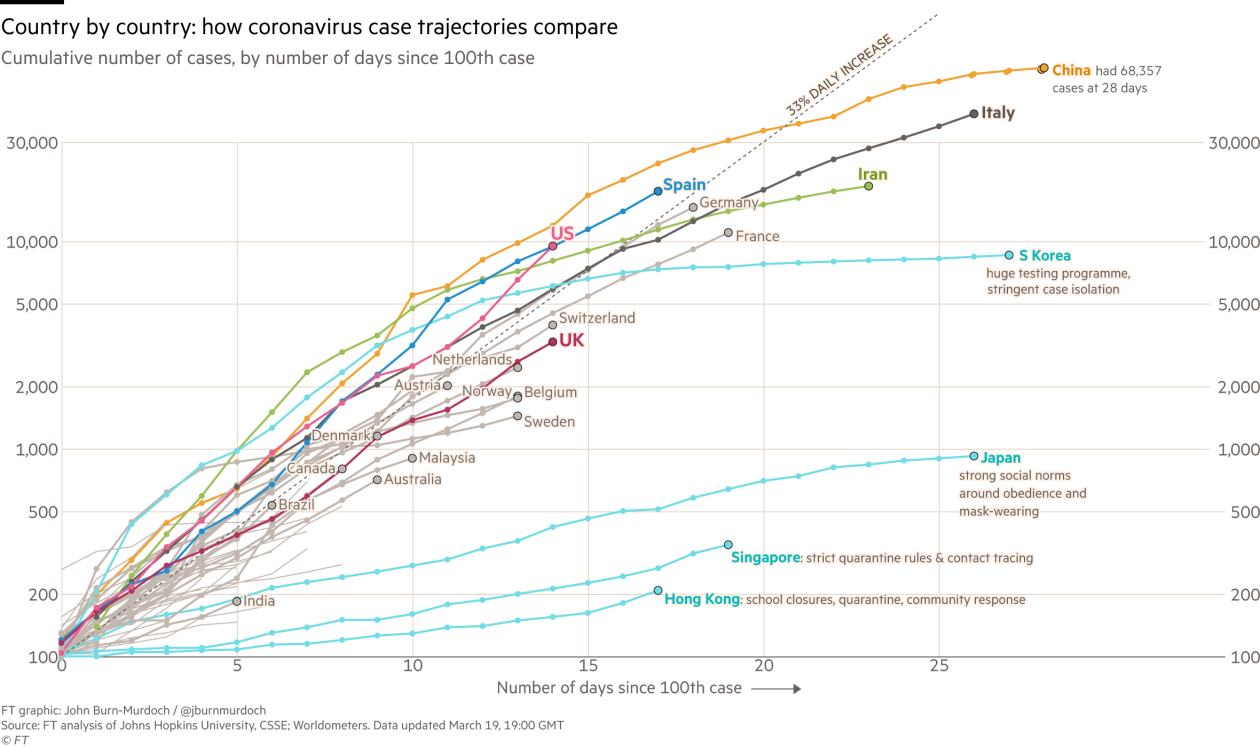
Figure 2: Check Financial Times for the live version of this figure.
For our UC Davis readers, find campus updates here.
California state updates can be found here.
CDC updates can be found here.
WHO updates can be found here.
Resources:
The WHO daily situation reports.
Cohen, J.; Powderly, WG. Infectious diseases. 2nd edn.. Mosby; New York: 2004.
de Wilde, Adriaan H., et al. “Host factors in coronavirus replication.” Roles of Host Gene and Non-coding RNA Expression in Virus Infection. Springer, Cham, 2017. 1-42.
de Wit, Emmie, et al. “SARS and MERS: recent insights into emerging coronaviruses.” Nature Reviews Microbiology 14.8 (2016): 523.
Li, Yan‐Chao, Wan‐Zhu Bai, and Tsutomu Hashikawa. “The neuroinvasive potential of SARS‐CoV2 may be at least partially responsible for the respiratory failure of COVID‐19 patients.” Journal of Medical Virology (2020).
Paules, Catharine I., Hilary D. Marston, and Anthony S. Fauci. “Coronavirus infections—more than just the common cold.” Jama 323.8 (2020): 707-708.
*A cordon sanitaire is the establishment of a quarantine zone where both sick and healthy people are not allowed to leave.

