Written by: Sydney Wyatt
Edited by: Hongyan Hao
How nutrigenomics and other genetic information contribute to personalized health in the age of direct-to-consumer genetic testing.
Nutrition has long been touted as a disease-fighting tool. Vitamin C supplements cure scurvy. Diets low in phenylalanine, an amino acid found in protein and some artificial sweeteners, keep phenylketonuria patients’ symptoms at bay. The ketogenic diet was invented to treat epilepsy. However, some of these tools have taken on new, sometimes inaccurate, benefits and companies have exploited these perceived benefits, profiting off of misinformed consumers. A popular example is the use of vitamin C to prevent or cure the common cold. There is no evidence to support this claim, yet the companies behind Airborne and Emergen-C profit off this misguided belief.
That being said, nutrigenetics and nutrigenomics aim to treat and manage genetic diseases like phenylketonuria that rely heavily on dietary adjustments to ease symptoms. However, there is a push to leverage these fields for personal health regardless of disease. With the increase of direct-to-consumer (DTC) genetic testing — 23andMe, AncestryHealth, Orig3n, Helix, etc. — consumers have access to genetic information about their risk of certain diseases and, based on self-reported information on their lifestyle, can get insight as to how these factors play into pre-existing genetic conditions. This information can be powerful, but making changes without a physician’s guidance “may harm the consumer’s health and finances.” Combine this with anecdotal evidence of certain diets managing cancer risk and symptoms, and nutrigenomics can quickly become unreliable at the consumer level.
Nutrigenomics complements the precision medicine movement by attempting to understand genetic responses to diet and leveraging that information to improve dietary guidelines. Hundreds of studies have attempted to demonstrate gene-lifestyle interactions for obesity and type 2 diabetes, but they had many limitations. For instance, these studies had small sample sizes that were inadequate for statistical analysis and relied on imprecise self-reported dietary and lifestyle data. Recent efforts to replicate the reported findings have failed, therefore the conclusions are unreliable at best.
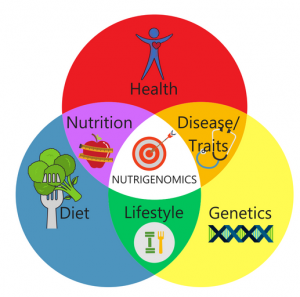
A number of factors contribute to health. If these are not properly balanced, there can be negative consequences. This illustrates how important it is to investigate more than just genetics and genomics when creating personalized health plans.
DTC genetic tests using a single locus to evaluate disease risk are not considered medically actionable. As a result, consumers can jeopardize their health by making changes based on this information. Famously, 23andMe received a letter from the US Food and Drug Administration (FDA) in 2013 expressing serious concerns over the results the company provided. The FDA claimed there was too much room for error when testing for diseases like breast cancer using a single locus (BRCA):
“Some of the uses … are particularly concerning, such as assessments for BRCA-related genetic risk and drug responses … because of the potential health consequences that could result from false positive or false negative assessments for high-risk indications such as these. For instance, if the BRCA-related risk assessment for breast or ovarian cancer reports a false positive, it could lead a patient to undergo prophylactic surgery, chemoprevention, intensive screening, or other morbidity-inducing actions, while a false negative could result in a failure to recognize an actual risk that may exist.”
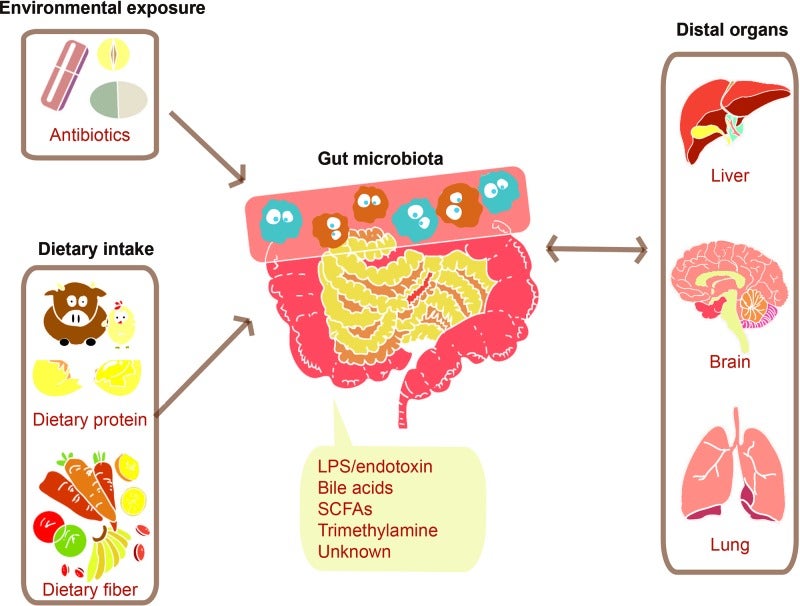
Environmental factors and diet can change the gut microbiome. This can have many effects on distal organs.
The letter continues to explain that consumers may self-manage treatment based on drug response testing with potentially deadly consequences. In the years since, 23andMe has received FDA approval to provide genetic information such as BRCA1/2 breast cancer risk, MUTYH-associated colorectal cancer risk, type 2 diabetes, and Parkinson’s disease. The majority of the test results consist of ancestry and trait reports, which have no medical relevance.
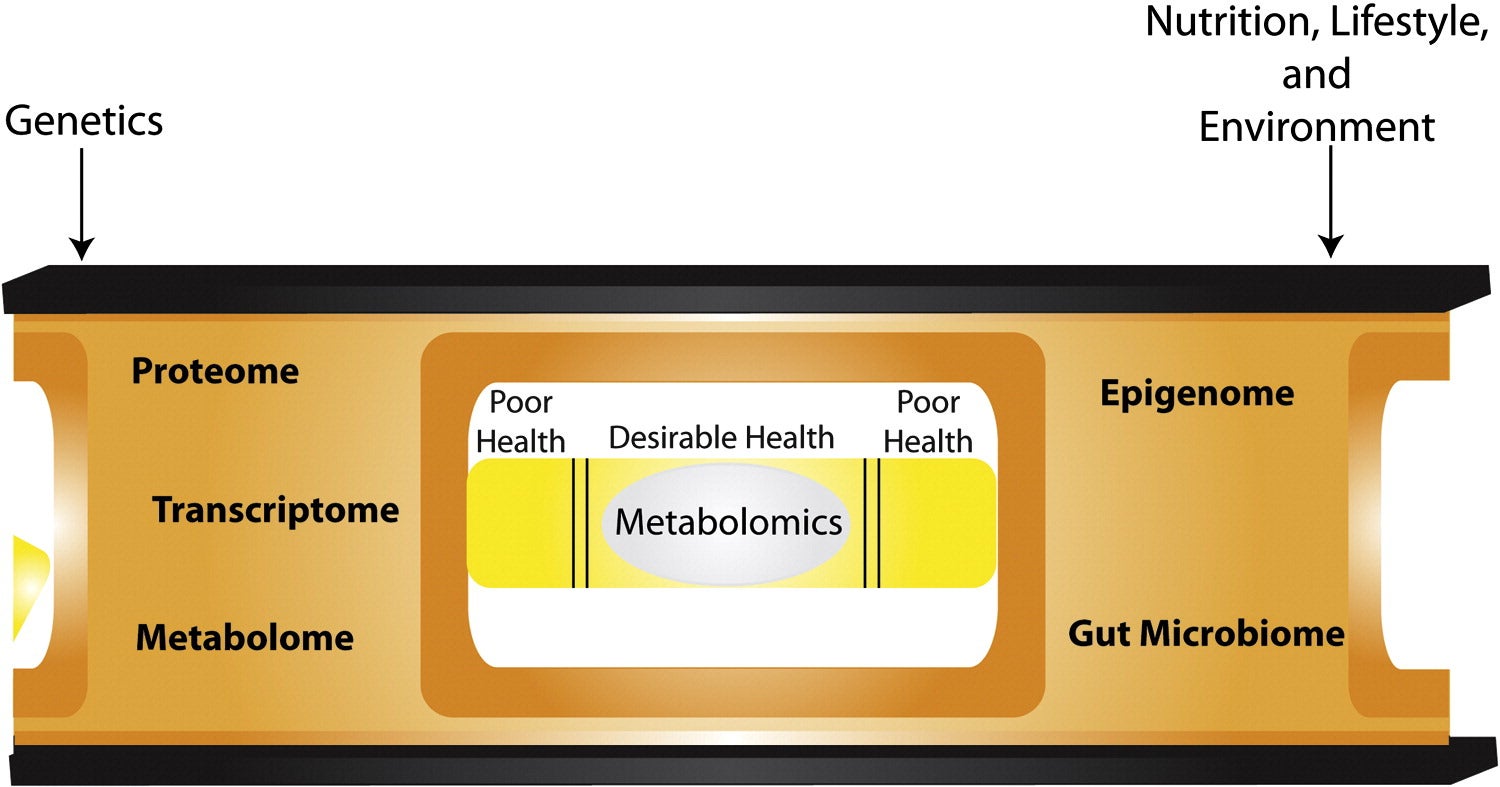
There are too many unknowns for a consumer to DIY a personalized nutrition plan based on their genetic test results alone. However, discussing the results in conjunction with factors such as family medical history and current health status with a physician is a safer way to personalize health. There are other “omics” that can provide more comprehensive information for health management strategies than genomics and nutrigenomics. Metabolomics and gut microbiota analysis offer promising insight into human health. Genetics and the environment can affect metabolism and gut flora composition, so this provides downstream information. Nutrigenomics still has a leg up on these techniques with regards to accessibility and affordability, but there may be a future where these analyses will be part of a routine check-up. Until then, take your test results with a grain of salt and consult your physician before making major changes to your lifestyle.
Bibliography:
- Phenylketonuria (PKU). (2018, January 27).
- D’Andrea Meira, I., Romão, T. T., Pires do Prado, H. J., Krüger, L. T., Pires, M. E. P., & da Conceição, P. O. (2019, January 29). Ketogenic Diet and Epilepsy: What We Know So Far.
- Gunnars, K. (2014, June 17). 20 Mainstream Nutrition Myths (Debunked by Science).
- Marshall, M. (2019, October 2). No, Vitamin C won’t cure your cold.
- Sommer, C. (2019, June 13). Food as medicine? Scientists are getting closer through nutrigenomics.
- Ordovas, J. M., Ferguson, L. R., Tai, E. S., & Mathers, J. C. (2018, June 13). Personalised nutrition and health.
- Metcalf, E. (2018, January 5). Photo Gallery: 10 Top Foods to Fight Cancer.
- Stern, A. P. (2019, June 17). Feeding the Beast: Could Eating the Right Diet Starve Cancers Like Mine?
- Li, S. X., Imamura, F., Ye, Z., Schulze, M. B., Zheng, J., Ardanaz, E., … Wareham, N. J. (2017, July). Interaction between genes and macronutrient intake on the risk of developing type 2 diabetes: systematic review and findings from European Prospective Investigation into Cancer (EPIC)-InterAct.
- Guasch-Ferré, M., Dashti, H. S., & Merino, J. (2018, March 1). Nutritional Genomics and Direct-to-Consumer Genetic Testing: An Overview.
- Dickey, M. R. (2013, November 25). The FDA Wants 23andMe To Stop Marketing Its Genetic Testing Kits.
- McNiven, E. M. S., German, J. B., & Slupsky, C. M. (2011, October 12). Analytical metabolomics: nutritional opportunities for personalized health.
- Cheng, M., Cao, L., & Ning, K. (2019, October 9). Microbiome Big-Data Mining and Applications Using Single-Cell Technologies and Metagenomics Approaches Toward Precision Medicine.