Written by: Devan Murphy
Edited by: Jennifer Baily
Due to the pandemic, most of us are spending more time in front of our screens. Honestly, I spend a lot more time on social media than I used to, and it has affected my mental health. No, it isn’t the dreaded FOMO (fear of missing out). It’s the posts from some of my friends and family that have shattered my perception of the people I thought I knew. As I scroll, I see an accumulation of conspiracy theories about COVID, unwillingness to help protect others by wearing a mask in public, and little empathy or consideration for the essential workers and medical professionals putting their life on the line while we sit at home. Although the internet is a valuable tool with a wealth of information and a method for connecting people, it can also be used for the complete opposite—disseminating falsehoods and driving a wedge between communities.
This weighs heavy on my mind and heart as people who helped raise me and shape who I am today share and legitimize misinformed views on the pandemic. But the information they insist on propagating results in behavior that goes against the very values I learned growing up. To see them posting harmful opinions and incorrect information feels like an attack on my profession. As a student in the Veterinary Student Training Program, I reside at an interface between the medical and basic science fields. To me, this situation is similar to clients who come into the clinic, ignore your professional opinion, and insist on telling you how to do your job because Dr. Google diagnosed their pet’s ailments for you. In the light of COVID, research scientists are now getting a taste of this frustration dealing with a population that is either ignorant or belligerently dismissive of facts (although climate change scientists have known this pain for a while now).
I do understand how the public could be confused. There is SO MUCH information out there, but this is what we deal with in science all the time. And as graduate students, I think we are exceptionally good at updating our point of view when we receive new data. I remember a conversation with a family member about grocery bags. He was annoyed about paper bags being brought back into fashion. It went something like this:
I don’t understand. We used to use paper bags, then they told us not to cut down trees, so we all switched to plastic. Now, everything is “Plastic is bad, plastic is ruining this environment.” So, which is it? We are supposed to go back to killing trees?
I tried to explain that as we get new information, we need to reimagine our behaviors. It is natural for scientists to understand that nothing is simple. There are always things we don’t know; we live on the frontier of the known and undiscovered. As we find new information and uncover confounding variables, we build them into our understanding or understand when to reject them. I wish it was easy as a superhero movie, where the bad guy is easily identifiable. But that’s not the real world. It is messy and problems are multifactorial, and clear straightforward solutions rarely exist. But here is the irony, in this situation, a common enemy does exist! Coronavirus. So, with a clear threat in sight, why are some people insistent on defying health experts instead unifying to defeat the pandemic?
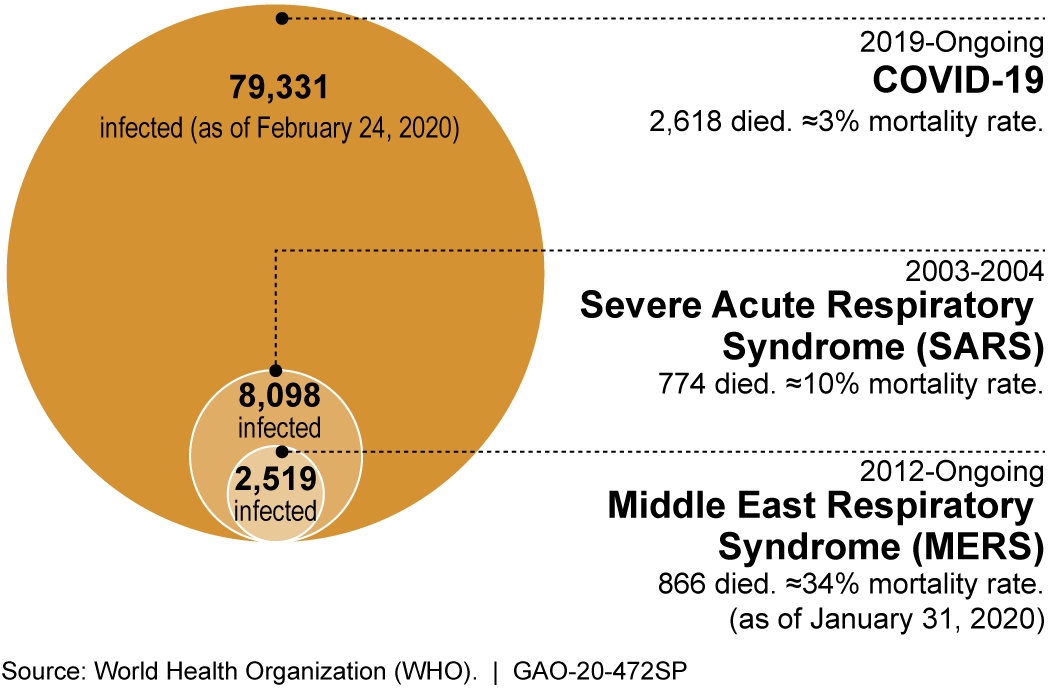
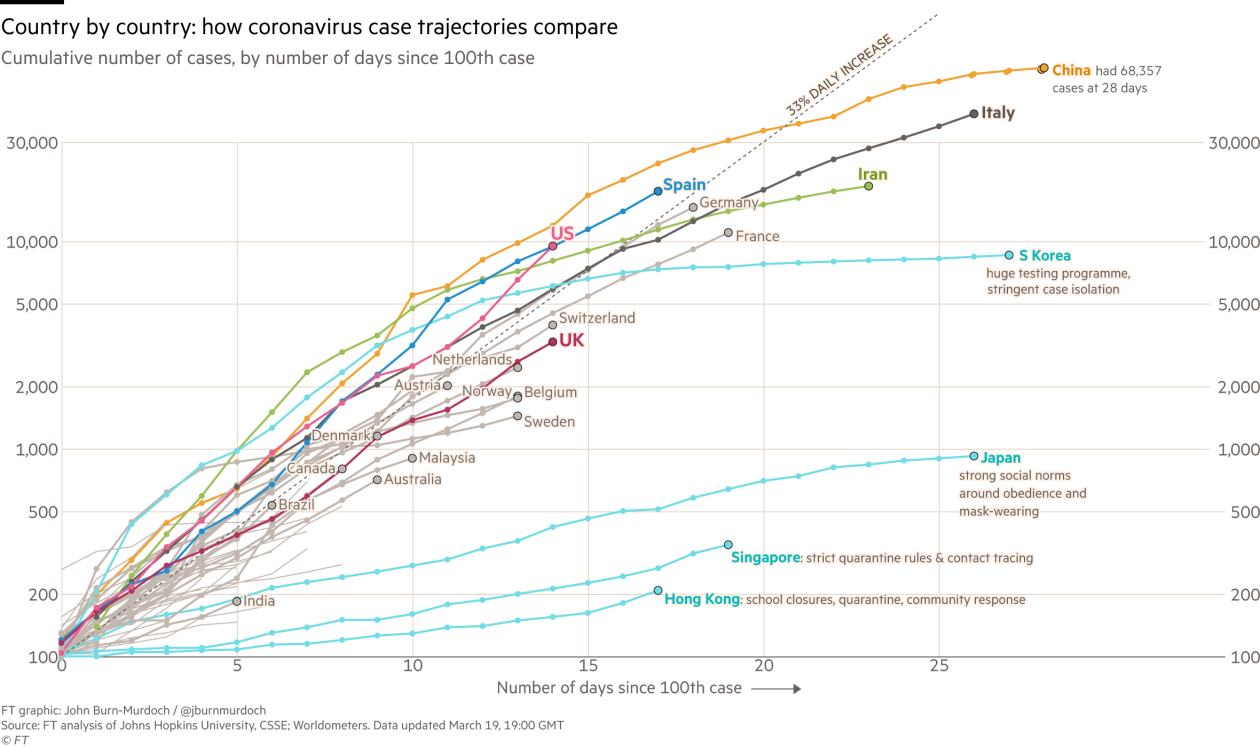
Initially, who knew what to do? Wear a mask, don’t wear a mask? And unfortunately, with government leaders not always being the most reliable sources, downplaying the severity of the problem and being slow to take action, it can be very confusing for someone watching the news to know what actions to take. However, now it is clear this virus is very contagious, deadly, and masks help prevent transmission. Therefore, perpetuating misinformation and bashing public health guidelines is a safety concern.
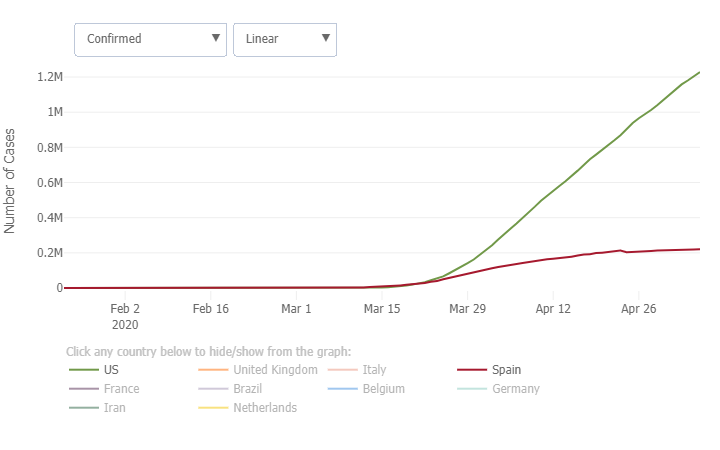
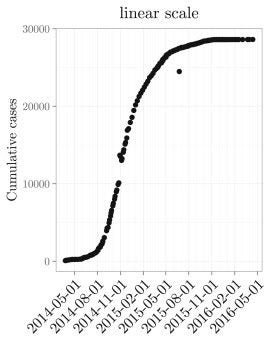
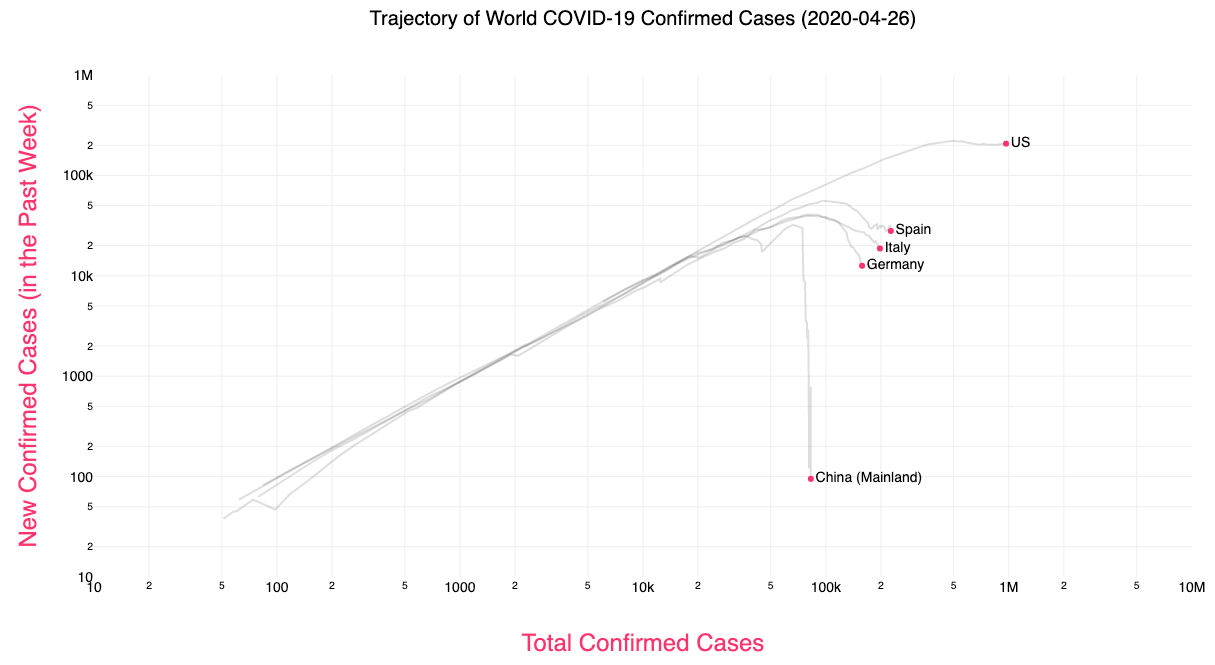
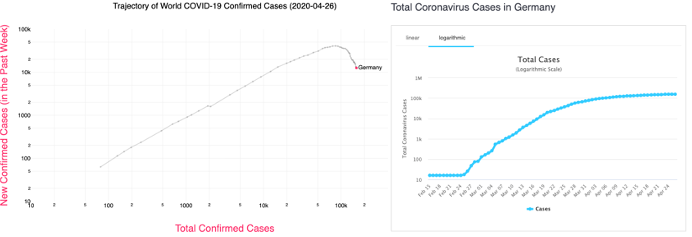
So, as graduate students, a community versed in critical thinking and evaluating primary literature, is it part of our job to combat misinformation online? Is it our place? And what internal conflict does this pose to call out our family members or friends? Interestingly, I wanted a career in science because I thought it was the unbiased pursuit of facts, untainted by the subjectivity of the humanities. Why deal with people when numbers don’t lie. But numbers can lie. In the worst case, they are purposely manipulated(1), but even in the best of circumstances, statistics without context mean nothing. And without placing these numbers in the proper context, it is easy to misdirect the audience. As recent events have made perfectly clear, science is not devoid of these conflicts. Our science is funded by taxpayers to help the public, therefore, getting involved to make science interpretable and usable to the public is implied in that paycheck.
Leaders and officials seem to be catching up on the relevance of internet accountability. The United Nations started an initiative to provide reliable information about COVID(2) and some social media sites like Twitter began fact checking posts(3). But to do this, you need to critique the information. Scientists do this all the time with peer review, disclosing conflicts of interest, and discussing the limitations of their work. However, it takes time to go through and fight/debunk all of the misinformation. In contrast, it takes NO effort to make stuff up to support a false narrative. I’m lucky enough to still have my job, and I honestly don’t have the time to refute all the misinformation I come across. To some extent, it must be the responsibility of the individual to self-educate. Again, there is a wealth of information online.
While I strive to stress the importance of accountability online, I acknowledge that this may not be an entirely safe conversation as people feel attacked when you dispute their worldview. So much of science has been tied to politics, which becomes emotional quickly. Being rejected or cut off by loved ones may not be an option. But if possible, in the way that personally works best for you (1-on-1 conversations, public sharing of valid resources, etc.), I think we have some responsibility as a science community to stop the spread of misinformation. That doesn’t mean everyone will listen, but letting this information spread unchallenged, like the virus, is dangerous.
(For more information, about spotting misinformation and fighting it, check out Fleming’s article (4) )
- Florida and Georgia facing scrutiny for their Covid-19 data reporting – CNN. https://www.cnn.com/2020/05/20/us/florida-georgia-covid-19-test-data/index.html.
- Online training as a weapon to fight the new coronavirus. https://www.who.int/news-room/detail/07-02-2020-online-training-as-a-weapon-to-fight-the-new-coronavirus.
- Twitter fact-checks tweets linking 5G and coronavirus – Business Insider. https://www.businessinsider.com/twitter-factchecks-tweets-5g-coronavirus-2020-6.
- Fleming, N. Coronavirus misinformation, and how scientists can help to fight it. Nature 583, 155–156 (2020).